Sun damage shows up everywhere. Fine lines around the eyes, dark spots scattered across cheekbones, that leathery texture that no amount of moisturizer seems to fix. Most treatments focus on covering symptoms rather than fixing what ultraviolet radiation actually breaks at the cellular level. But polydeoxyribonucleotide (PDRN) works differently because it targets DNA repair mechanisms directly, addressing photoaging where it starts. If you’re new to this ingredient, start with our complete guide to PDRN for foundational knowledge.
The science behind this approach centers on adenosine receptor activation and cellular regeneration pathways. When UV light damages skin cells, it doesn’t just create surface problems. It disrupts DNA, breaks down collagen matrices, and triggers inflammatory cascades that accelerate aging. PDRN intervenes in these processes through mechanisms that researchers are still mapping out, though the clinical results have pushed it into mainstream dermatology faster than most regenerative treatments.
Photoaging represents cumulative damage from years of sun exposure. Different from natural aging.
How UV Radiation Actually Damages Skin
Ultraviolet light penetrates the epidermis and reaches the dermis where collagen and elastin fibers provide structural support. UVA rays (the ones that pass through windows and clouds) cause direct DNA damage to fibroblasts, the cells responsible for producing new collagen. UVB rays trigger inflammation and oxidative stress that compounds the problem. Over time, this creates visible changes most people associate with aging but stem directly from sun exposure.
Fibroblasts slow down. Collagen production drops. The extracellular matrix weakens and skin loses its ability to bounce back from daily stress. Melanocytes (pigment-producing cells) start behaving erratically, creating uneven tone and persistent dark spots that resist typical brightening treatments. And the repair mechanisms that normally fix DNA damage become overwhelmed, letting mutations accumulate.
This explains why photoaged skin looks and behaves so differently from naturally aged skin. The damage runs deeper than wrinkles. For a critical examination of what the research actually shows, see our analysis of PDRN efficacy and the data behind the claims.
PDRN’s Mechanism for Cellular Repair
PDRN consists of DNA fragments extracted from salmon or trout sperm cells, processed into chains of nucleotides that mammalian cells recognize and respond to. When injected into damaged skin, these fragments bind to adenosine A2A receptors on cell surfaces. This binding triggers several repair pathways simultaneously.
First, it stimulates fibroblast proliferation. Cells that had slowed their collagen production start ramping up again, synthesizing new structural proteins. Research shows PDRN activates growth factors and enhances cellular metabolism, essentially waking up dormant repair systems. Second, it modulates inflammation by reducing pro-inflammatory cytokines that keep damaged tissue in a chronic state of stress. Third, it promotes angiogenesis (new blood vessel formation), improving nutrient delivery to compromised areas.
But the DNA repair aspect matters most for photoaging. PDRN provides nucleotide building blocks that cells use to patch damaged DNA strands. While it doesn’t replace professional sun protection or undo decades of damage overnight, it gives cells resources to repair themselves more efficiently than they could alone.
Think of it as providing both the construction materials and the work crew.
Collagen Restoration in Sun-Damaged Tissue
Collagen degradation shows up as sagging, deep wrinkles, and loss of facial volume. UV exposure activates matrix metalloproteinases (MMPs), enzymes that break down collagen faster than fibroblasts can replace it. This creates a deficit that accumulates over years.
PDRN addresses this through multiple angles:
- Fibroblast activation: Stimulating dormant cells to resume collagen synthesis at rates closer to younger skin
- MMP inhibition: Reducing the enzymatic breakdown that keeps collagen levels depleted
- Growth factor upregulation: Increasing production of TGF-beta and VEGF that support tissue remodeling
Clinical observations show texture improvements within weeks, though significant structural changes require months of treatment. The dermis needs time to rebuild what took years to break down. Patients typically notice reduced fine lines first, followed by improved skin thickness and resilience. Deep wrinkles respond more slowly because they involve more severe architectural damage.
Real collagen restoration beats temporary fillers for functional improvement. Skin that produces its own structural proteins maintains better hydration, responds better to other treatments, and ages more gracefully going forward.

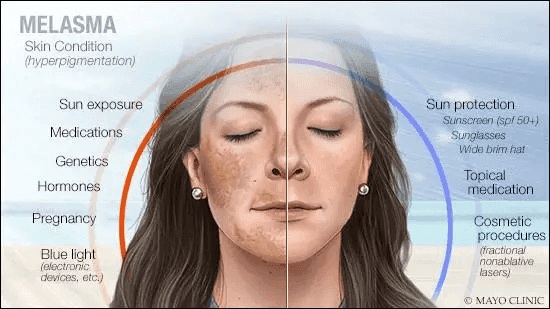
Targeting Hyperpigmentation From UV Exposure
Sun spots, melasma, and uneven tone result from melanocyte dysfunction triggered by chronic UV damage. Normal melanin production involves controlled response to sun exposure. Photoaged melanocytes lose this control, producing excess pigment in irregular patterns that persist even without continued sun exposure.
Studies demonstrate PDRN’s effects on pigmentation when combined with other compounds, showing modulation of nuclear factor erythroid 2-like 2 (Nrf2) pathways involved in oxidative stress responses. This matters because oxidative stress drives melanocyte hyperactivity. By reducing cellular stress, PDRN helps normalize melanin production without completely suppressing it.
Pigmentation changes take longer than collagen effects. Melanin already deposited in skin needs to cycle through natural turnover, which happens over weeks to months. PDRN doesn’t bleach existing pigment but prevents new excessive production while supporting even tone distribution. This creates gradual, natural-looking improvements rather than dramatic overnight changes.
Combining PDRN with vitamin C serums or niacinamide often accelerates results. The cellular repair PDRN provides makes skin more responsive to topical treatments that target pigment pathways directly. For detailed protocols on pigmentation treatment, explore our guide on PDRN and hyperpigmentation.
Clinical Applications and Treatment Protocols
Dermatologists typically administer PDRN through microinjections into affected areas, similar to mesotherapy techniques. The injectable form delivers concentrated doses directly to damaged dermis where it’s needed most. Treatment frequency varies based on damage severity and individual response.
Standard protocols involve:
- Initial phase: Weekly sessions for 4-6 weeks to jumpstart repair mechanisms
- Maintenance phase: Monthly treatments for several months to sustain collagen production
- Long-term management: Quarterly sessions to prevent regression
Some practitioners use microneedling to enhance PDRN penetration when treating broader areas like the full face, chest, or hands. The controlled injury from needling triggers additional wound-healing responses that synergize with PDRN’s regenerative effects—learn more about PDRN and microneedling results. Topical PDRN formulations exist but show less dramatic results because skin absorption limits how much reaches the dermis. Understanding PDRN absorption and bioavailability helps explain these limitations.
Response times differ significantly between patients. Younger individuals with moderate photoaging respond faster than those with decades of accumulated damage. Skin thickness, genetic factors, and continued sun exposure all influence outcomes.
Comparing PDRN to Other Photoaging Treatments
Retinoids remain the gold standard for photoaging because of extensive research backing their collagen-boosting and cell-turnover effects. They work through different mechanisms than PDRN, primarily by binding to retinoic acid receptors that regulate gene expression. Many dermatologists view PDRN and retinoids as complementary rather than competing treatments.
Laser resurfacing removes damaged outer layers and triggers healing responses that remodel deeper tissue. More aggressive than PDRN but also involves longer downtime and higher complication risks. Chemical peels work similarly by controlled destruction followed by regeneration.
PDRN offers gentler repair with minimal downtime. No peeling, no photosensitivity restrictions, no visible recovery period. This makes it attractive for patients who can’t take time off for more intensive procedures or those seeking gradual improvements without dramatic intervention. For practitioners interested in offering these treatments, our PDRN training courses guide covers certification requirements.
The biological approach differs fundamentally from ablative methods. Rather than forcing skin to regenerate through injury, PDRN supports natural repair mechanisms that already exist but need enhancement. Some evidence suggests this produces more sustainable results because it strengthens tissue rather than temporarily shocking it into production mode.
Evidence Base and Research Findings
Studies examining PDRN’s molecular mechanisms confirm its effects on multiple aging pathways, including antioxidant defense systems, collagen synthesis markers, and inflammatory mediators. In vitro research shows PDRN protecting fibroblasts from UV-induced damage when applied before or after exposure. Animal models demonstrate accelerated wound healing and improved tissue quality in UV-damaged skin treated with PDRN compared to controls.
Human clinical trials remain limited compared to more established treatments, though published case series show consistent improvements in photoaging markers. Most studies evaluate PDRN combined with other treatments rather than as monotherapy, making it difficult to isolate its specific contribution. This reflects real-world practice where dermatologists typically integrate PDRN into comprehensive anti-aging protocols.
The adenosine receptor mechanism provides theoretical backing for observed effects. A2A receptor activation influences numerous cellular processes relevant to photoaging, from inflammation control to tissue remodeling. This receptor-mediated approach differs from many topical treatments that work primarily through antioxidant effects or surface exfoliation.
More research would help establish optimal dosing protocols, identify which patient populations benefit most, and clarify long-term effects of repeated treatments. Current evidence supports PDRN’s role in photoaging treatment while acknowledging gaps in understanding precise mechanisms and ideal application methods.
Practical Considerations and Expectations
Cost varies significantly by provider and geographic location. Most insurance plans classify PDRN treatments as cosmetic, leaving patients responsible for full payment. Multiple sessions required for meaningful results increase total investment compared to single-procedure options.
Side effects remain minimal for most patients. Temporary injection-site reactions like redness, mild swelling, or bruising resolve within days. Allergic reactions to salmon-derived PDRN are theoretically possible but rarely reported. The biological origin means PDRN integrates with human tissue without triggering foreign-body responses that synthetic materials sometimes cause.
Patients need realistic timelines. Collagen production takes months to translate into visible structural changes. Those expecting immediate dramatic results will feel disappointed. But individuals willing to commit to treatment series and understand the gradual nature of regenerative medicine typically report satisfaction with outcomes.
Continued sun protection remains non-negotiable. PDRN repairs existing damage but can’t prevent new damage from ongoing UV exposure. Daily broad-spectrum sunscreen, protective clothing, and avoiding peak sun hours protect treatment investments and prevent canceling out improvements with fresh photoaging.
Integration With Comprehensive Skin Protocols
Dermatologists rarely use PDRN alone because photoaging involves multiple simultaneous processes requiring different interventions. Common combinations include:
- Topical retinoids: For continued cell turnover and collagen stimulation between PDRN sessions
- Antioxidant serums: Vitamin C, vitamin E, ferulic acid to neutralize free radicals
- Hydration support: Hyaluronic acid and ceramides to maintain barrier function
- Chemical exfoliants: Gentle acids to remove damaged surface cells and improve product penetration
Some practitioners layer PDRN with platelet-rich plasma (PRP), another regenerative treatment using the patient’s own growth factors. The theory suggests combining different biological signals creates synergistic repair responses. Whether this produces better results than either treatment alone remains debated, though many patients pursue combination approaches.
Microneedling sessions often incorporate PDRN as the solution applied during or immediately after needling. The microchannels created by needles allow deeper penetration while the controlled injury amplifies regenerative signaling. This combination has gained popularity for treating severe photoaging across larger areas like the chest and hands where injectable treatments become impractical.
Who Benefits Most From PDRN Treatment
Ideal candidates show moderate photoaging without extreme damage requiring more aggressive intervention. Fair-skinned individuals who accumulated significant sun damage in youth but haven’t yet developed severe wrinkling or laxity respond particularly well. Those seeking preventive treatment in early photoaging stages may also benefit from supporting cellular repair before visible damage becomes pronounced.
People with active skin conditions like rosacea, eczema, or psoriasis need careful evaluation before starting PDRN. While it generally proves gentle, any injectable treatment can potentially flare inflammatory conditions. Immunocompromised patients require additional consideration given PDRN’s immune-modulating effects.
Realistic expectations separate satisfied patients from disappointed ones. PDRN won’t erase decades of sun damage or replace surgical intervention for severe laxity. It improves tissue quality, supports natural repair, and can prevent further deterioration when combined with proper protection. Those viewing it as one component of long-term skin health rather than a miracle cure report better experiences.
Moving Forward With Photoaging Treatment
Photoaging reversal requires patience and commitment to ongoing skin health. PDRN represents a biological approach that works with cellular repair mechanisms rather than forcing changes through destruction and regrowth. The DNA-based repair pathway offers unique advantages for sun-damaged tissue struggling to maintain normal function. For a comprehensive clinical perspective, read our practitioner’s overview of PDRN in aesthetic medicine.
Results accumulate slowly but tend to look natural because they stem from actual tissue regeneration rather than temporary interventions. Combining PDRN with sun protection, appropriate topical treatments, and healthy lifestyle factors creates the best environment for sustained improvement. No single treatment fixes complex photoaging, but supporting cellular repair through multiple angles produces meaningful changes.
Anyone considering PDRN should consult qualified dermatologists who can assess individual damage patterns and design appropriate protocols. The treatment continues evolving as research clarifies mechanisms and optimal applications. Early evidence suggests significant potential for reversing UV damage at cellular levels that other treatments don’t adequately address.

